The lawsuit was filed in 2018 by a group of Republican state Attorneys General. They argued that after the Republican-controlled Congress enacted tax reform in 2017 and changed the Individual Mandate penalty to zero, this keystone ACA provision was now unconstitutional. Without the Individual Mandate, their argument continued, the pre-existing conditions provisions of the ACA were invalid as well. The Individual Mandate had required everyone to purchase health insurance or pay a penalty. The lawsuit grounded its claim in the U.S. Supreme Court decision upholding the Individual Mandate in 2012 as a tax. Since the tax penalty was changed to zero, the constitutional foundation of the ACA was gone, according to the suit.
It was an argument that many legal experts believed was weak and going nowhere. But U.S. District Judge Reed O’Connor in Fort Worth, Texas agreed with the plaintiffs in late 2018, finding the Individual Mandate unconstitutional, and that the rest of the law could not stand without it. A three-judge panel from the Fifth Circuit Appeals court split on whether to uphold the ruling in December 2019. Instead the Appeals Court ordered the matter be returned to O’Connor who was to use a “finer-toothed comb” to determine what ACA provisions could stand even without the Individual Mandate. With the U.S. Supreme Court denying the request for expedited review, legal experts believe it could take at least another year before the case completes it run through the lower courts.
ACA gains bi-partisan support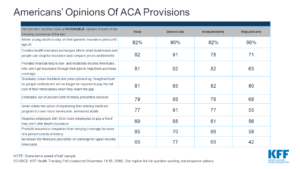
This third challenge of the ACA comes at a time when bi-partisan support for many provisions of the healthcare law has grown. Healthcare is a high-priority issue for many Americans. A recent Gallup poll found that 43% of U.S. households report pre-existing conditions. Before the ACA, health insurance companies could refuse to cover pre-existing conditions or charge more to provide coverage. More than half of respondents to a Kaiser Family Foundation Tracking Poll say they’re worried that they or someone in their family will lose health insurance coverage if the Supreme Court overturns the ACA.
New Jersey recently passed laws that would keep key ACA provisions in place even if the Supreme Court strikes down the law. And California now offers subsidies to people whose earnings are too high to qualify for federal tax credits to buy health coverage through the state’s ACA insurance exchange.
How has the ACA impacted America’s health and healthcare system?
More than 20 million people have gained health coverage because of the ACA. Across all demographic groups, uninsured rates have fallen dramatically. The 37 states that accepted federal Medicaid expansion dollars not only increased their insured population, but also improved access to care while reducing uncompensated care costs. The latest figures still show that 27.9 million people remain uninsured, but this number is far lower than the 46.5 million uninsured before the ACA became law in 2010.
The ACA has not only provided healthcare to those who had previously done without, but also brought about improvements for all healthcare consumers.
Under the ACA, all health care plans must:
- Allow adult children to stay on a family health plan up to age 26;
- Cover those with pre-existing conditions and cannot charge higher premiums;
- Provide preventive services with no out-of-pocket costs;
- Have no lifetime or annual dollar limit on essential health benefits such as hospitalization, prescription drugs, maternity and newborn care; mental and behavioral health treatment;
- Spend 85 cents of every dollar directly on care (companies with more than 50 employees);
- Not charge rates based on gender.
Can the ACA survive without the Individual Mandate?
The rationale behind the ACA’s Individual Mandate was to ensure that enough healthy people participated in the program. In doing so, risk could be spread out broadly and keep premiums low for everyone, even those with expensive medical conditions. But what’s actually happened is that even without the mandate, healthy people are not opting out. Rather, the availability of income-based subsidies seem to have a stronger effect on keeping people in the health care insurance markets. While premiums in the individual market rose in the early years of the ACA, they are declining by an average of 4% in 2020. The number of health insurers offering plans in 2020 increased, bringing the total number to 175, the largest number of issuers since 2016.
The actual performance of the ACA health care insurance markets undercuts a central argument in the current court challenge to the ACA. Improvements in America’s healthcare system are still sorely needed, but pulling the plug on the ACA could have the same effect on healthcare delivery for millions of people.



