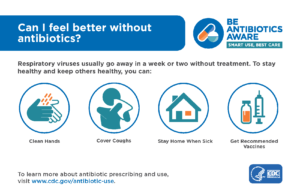
- Getting plenty of rest;
- Staying hydrated;
- Soothing symptoms such as congestion by drinking warm fluids and adding moisture to the air;
- Taking over-the-counter (OTC) cold and cough medications to help relieve symptoms. Get medical advice before giving a child OTC cold medicines, as some ingredients are not recommended for them.
Certainly, antibiotic drugs have saved countless lives, beginning with this compelling story. In 1942, Mrs. Anne Miller of New Haven, Connecticut was close to death due to infectious germs that had invaded her bloodstream. Desperate to save her, doctors gave her an experimental drug: penicillin, which had been discovered just 14 years earlier. Within hours she recovered, becoming the first person in the world to be saved by an antibiotic. Rather than dying in her thirties, Mrs. Miller lived to be 90 years old.
Now fast forward to 2005. Chris Linaman was recovering from ACL surgery after a basketball injury. Recovery was going well, and with doctor-approval Chris and his family took a vacation. But after a day at the water park, Chris’s leg became swollen, red, and hot to the touch. He went to the doctor and was diagnosed with a MRSA infection in his knee. Six months, five surgeries, and four antibiotics later, doctors at last found an antibiotic that started working. The trauma of feeling his body deteriorate, multiple emergency room visits, and his wife finally being told that if the infection travelled to his brain Chris could die, was shocking to the entire family. It drove home the reality that antibiotic resistance could indeed be a killer.
What’s happened since the remarkable 1942 antibiotic cure and the current day crisis of antibiotic resistance?
Over two million Americans get antibiotic resistant infections every year. At least 23,000 people die from them. Anyone can get this type of infection, and it can start with something as simple as a cut or routine medical procedure.
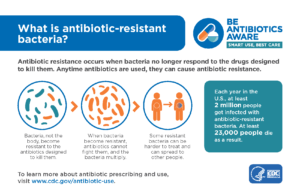
People don’t get resistant to antibiotics. Rather, bacteria can develop the ability to fend off the germ-killing power of antibiotics, thus leaving bacteria to grow and spread. When these resistant bacteria render antibiotics ineffective, we lose the ability to fight illnesses that were once easily treatable, and lead to even more dangerous infections.
How does bacteria become resistant to antibiotics?
While it’s not simple, the simple answer is that bacteria find ways to adapt and defend themselves against the antibiotic. Some bacteria genetically change to literally pump antibiotics out of their cell walls, or develop a defensive membrane to keep antibiotics from entering. The longer and more often antibiotics are used, the more adept bacteria become at fighting them off. So today, after decades of widespread antibiotic use, some bacteria no longer are killed off, forcing doctors to search for other antibiotic strains that have not yet become resistant to the bacteria.
What’s the answer to antibiotic resistance?
 It’s important to understand exactly what circumstances call for antibiotic use. We often use the words germs, bacteria, and viruses interchangeably, but there is a big difference. The broad term – germs, includes both bacteria and viruses. Antibiotics only kill bacteria, not viruses. Taking an antibiotic for an illness caused by a virus won’t help you get better. It does offer bacteria the chance to practice and increase resistance to the antibiotic. As Chris Linaman’s story demonstrates, this is no small problem. When antibiotics can no longer effectively combat illness-causing bacteria, we’re moving backward in time to the beginning of the 20thcentury when infectious diseases were major killers.
It’s important to understand exactly what circumstances call for antibiotic use. We often use the words germs, bacteria, and viruses interchangeably, but there is a big difference. The broad term – germs, includes both bacteria and viruses. Antibiotics only kill bacteria, not viruses. Taking an antibiotic for an illness caused by a virus won’t help you get better. It does offer bacteria the chance to practice and increase resistance to the antibiotic. As Chris Linaman’s story demonstrates, this is no small problem. When antibiotics can no longer effectively combat illness-causing bacteria, we’re moving backward in time to the beginning of the 20thcentury when infectious diseases were major killers.
So if this winter season has you sneezing, coughing and grabbing lots of tissues for a runny nose, don’t head for the doctor seeking an antibiotic cure. When a cold or flu hits, snuggle up with a warm cup of tea and do your best to minimize sharing those nasty cold germs. It will pass. Reversing antibiotic resistance will help ensure antibiotics will be effective when we truly need them.
The Centers for Disease Control (CDC) recommends seeking medical help if your illness lasts more than 10 days or if the symptoms are especially severe or unusual. A medical professional should also evaluate children younger than three months with a fever or are lethargic.